Synopsis
Despite digital pathology’s progress, whole slide imaging (WSI) and WSI-based digital pathology face slow adoption in surgical labs and intraoperative consultations due to critical challenges. These include workflow complexity from WSI integration, extended scanning times for intraoperative slides, prohibitive total case scanning times, risks from low-quality images, logistical issues managing large WSI files, limited regulatory approvals for WSI use during critical procedures like frozen sections, and the need for complex organizational changes. Overcoming these demands streamlined workflows, technological enhancements, regulatory adjustments, improved IT infrastructure, and comprehensive change management. These efforts are vital for integrating WSI effectively into surgical pathology and intraoperative care.
What Is Whole Slide Imaging?
WSI is an imaging technology that makes it possible to create a permanent digital representation of a physical specimen on a slide for later, purely virtual microscopic viewing. This allows you to perform virtual microscopy independent of time and location, eliminating the need to transport physical slides for examination.
Here are 7 reasons why pathology labs are not using WSI and WSI-based digital pathology to digitize their intraoperative consultations.
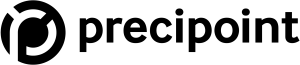
#1 – WSI Adds an Extra Step to the Workflow
Consultation during the intraoperative procedure is no race where split seconds are monitored; the general aim is to close cases within 20 minutes. However, time is always tight during intraoperative consultation. Adding a new step to the workflow can hardly be an option. Although WSI-based digital pathology eliminates the need to transport physical microscopy slides for examination, it, however, adds an extra step to the imaging process during which the slide needs to be digitized first using a slide scanner before it can then be viewed virtually using a viewer software.
#2 – Scanning a Single Intraoperative Slide Takes More Time
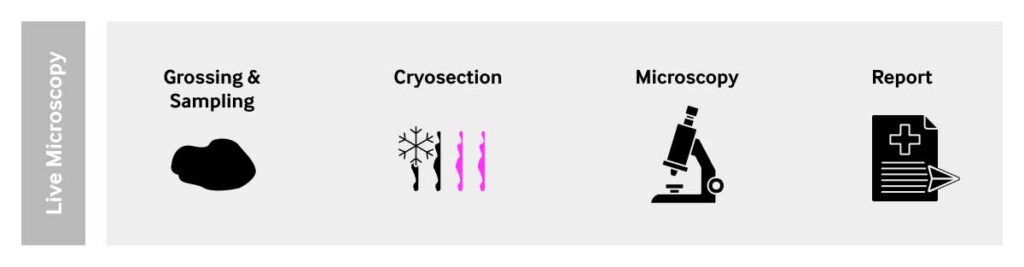
During surgery, sample preparation for microscopic assessment must be extremely fast. A slide is usually prepared manually within minutes. The frozen section procedure performs a rapid microscopic analysis of a specimen. In comparison, it takes hours to make a single glass slide using the FFPE procedure for sample preparation in routine pathology labs.
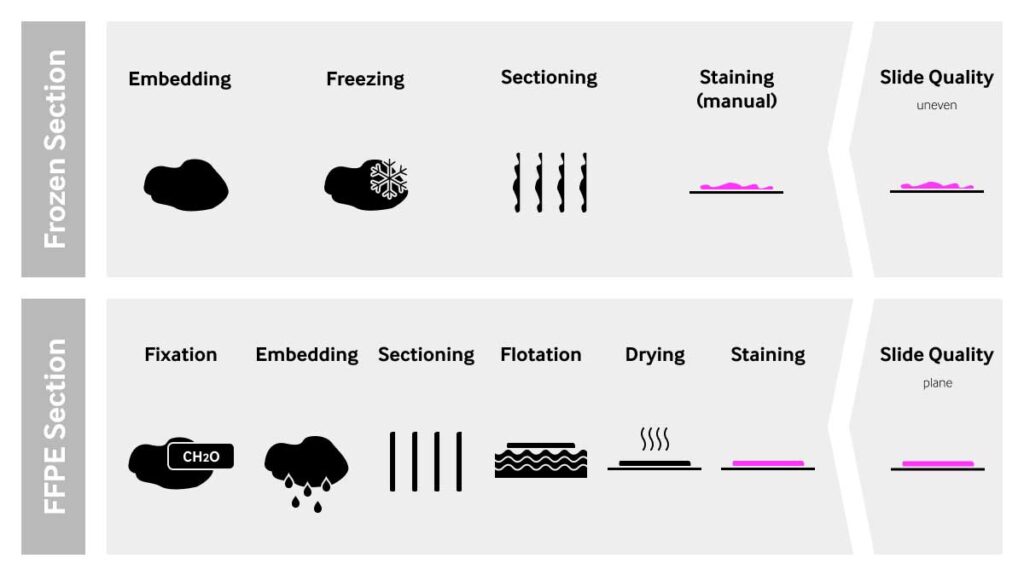
That difference in sample preparation methods has a very significant impact on microscopic imaging. While real-time imaging with microscopes, where users have live access to the specimen usually have no problem producing suitable images, digital scanners face very complex challenges. Uneven slides with a challenging sample topography require scanners to provide special scanning modes, or the use of z-stacking, for image acquisition. These scanning methods are much more time-consuming than the high-speed scan modes designed for FFPE slides. If high-speed scan modes are applied to uneven specimens, a lot of out-of-focus images will most likely be created.
As a result, scanning time for a single intraoperative slide takes on average 3 to 12 minutes, compared to 1 to 3 minutes for a standard FFPE slide. These values can vary significantly depending on several input variables. Yet, the ratio of time needed for scanning remains relatively unchanged.
The scan time for an intraoperative slide is about 3 to 4 times longer than a standard FFPE slide. That amount of time is generally not available during intraoperative procedures.

#3 – Total Scanning Time for the Entire Case is Prohibitive
Intraoperative cases usually consist of 3-4 glass slides per case. The total scan time for an exemplary case with 4 slides can add up to 48 minutes of scanning time per case.
It is obvious, that the additional process step introduced by WSI-based digital pathology will most probably not allow for intraoperative cases to be assessed within the given time frame of 15 to 20 minutes.

#4 – High Process Risks Due to Low-Quality Output Images
The quality of a sample has a direct impact on the scan time and the output image quality. The quality of a sample is largely determined by the sample preparation technique.
Quickly prepared frozen section slides have an uneven topography due to the natural challenges imposed by cutting frozen tissue. It usually contains many artifacts such as ice crystals and cutting artifacts. Smears often have overlapping layers of tissue or cells.
Due to the sample complexity, the output image when using WSI-based digital pathology is likely to contain unsharp images (out-of-focus) and may be very difficult to assess with accuracy. This can jeopardize the correct observation and interpretation of a virtual microscopy slide.
Given the time-sensitivity of intraoperative procedures, time-consuming rescanning is not an option as it could be in other applications such as routine pathology or research. Thus, WSI-based digital pathology introduces a significant new process risk.
#5 – Handling Gigantic WSI Images Out of Surgical Labs is a Big Challenge
Since WSI files are very large data files, with an average file size ranging from 500MB for histology slides to up to 2 GB for cytology slides, working with whole slide images comes with hefty requirements on the IT infrastructure.
A suitable IT network and storage infrastructure need to be in place to transfer these large files. The process of sending large files out for review by a remote specialist adds extra working steps and additional time to the workflow.
#6 – WSI Scanners Are Not Approved for Use During Frozen Section Procedures
In many countries, regulatory bodies have not approved WSI technology for use during intraoperative consultations. For example, the FDA specifies in their medical devices classification for whole slides imaging systems (product code PSY) states “the whole slide imaging system is not intended for use with slides prepared from frozen tissue, cytology, and non-FFPE hematopathology specimens (e.g., peripheral blood smear).”
#7 – Complex Management Change Needed to Implement WSI-based Digital Pathology Workflow
The adoption of WSI-based digital pathology for intraoperative procedures requires a project manager capable of managing a complex multi-stakeholder project and driving change at multiple levels:
The on-site technician likely needs to be retrained to achieve significant improvements in sample preparation quality to reduce scanning times. Pathologists need to be trained in using virtual microscopy, without the possibility of having any access to the live specimen. Solutions need to be found and implemented when the virtual images do not show the appropriate image quality. Quality management needs to get involved to design, run, and documenting self-validation. The process risks induced by the occurrence of blurry images and the introduction of an additional, time-intensive imaging process step will be key challenges to overcome adding another layer of complexity and costs. Lastly, the IT department needs to resolve the issue of handling extremely large WSI data sets in a short time frame.
Conclusion
Digitization of surgical pathology is far from trivial. The digitization of intraoperative consultations poses a different set of challenges than the ones commonly seen in routine pathology. The 7 reasons outlined in this article give an idea as to why WSI-based Digital Pathology may not be the best solution for digitizing intraoperative microscopic assessment. Thus, pathologists and pathology labs should look for alternatives and assess different solutions. However, companies such as PreciPoint are manufacturing state-of-the-art digital microscopes like the iO:M8 where there is no need to wait for Whole Slide Image (WSI)-scan slides. Additionally, it enables you to instantly assess the live microscopic images displayed on your screen.